
Dr Harry Singh details his approach to rejuvenating the temples and provides his considerations for those newer to injecting this area.
In a youthful face, the temples are full, convex, round or oval. As we age, this turns into a skeletal shape due to loss of temporal fascia, reduction in volume and the temporal fossa becoming more apparent and concave. One of the secondary effects is a loss of support for the eyebrows.1 This loss of volume is a result of the temporalis atrophies and the temporal fat pads decreasing, resulting in an undesirable, hollow appearance.1
Achieving a balanced and youthful appearance whilst counteracting volume loss can be achieved through dermal filler augmentation.2 Some facial manifestations of ageing reflect the combined effects of gravity, progressive bone resorption, decreased tissue elasticity and redistribution of subcutaneous fullness.3 Fat may reposition or shift within facial compartments due to gravity, causing an inferomedial displacement of the overlying skin envelope. This movement increases hollows in the cheeks and flattens the angles of the face.4
There are several changes in facial structures as we age. Bones remodel in specific areas, ligaments increase in laxity, the fat deflates, muscles decrease in mass and there is also tonus change, with the skin experiencing gradual laxity increase.5 As a result, faces present with an increased visible vasculature, lateral orbital rim, and upper zygomatic arch as well as a descent of the eyebrow tail.6
In this article, I will be discussing the different protocols I like to implement in my clinic for treating temple hollowness.
Most patients will be unaware of a loss of volume in the temple area and the effect this has on the attractiveness of the face. The ageing process can alter the symmetrical and balanced facial features found in youth. This impacts a patient’s physical attractiveness but also their self-esteem.7
In addition to the generic consultation questions, I will also ask specific questions and make personalised assessments based on the patient. I will compare the patient’s pre-treatment photos of the temporal area with a set of photos from a patient I’ve treated with temple filler and ask the patient to ‘spot the difference’. It is imperative that the patient can see in themselves the temple deformity. Then, during the assessment, I’ll get the patient to clench their teeth and feel for any hypersensitivity in the temporal muscle and warn of any potential chewing issues post-treatment.
As well as general contraindications for treatment such as active infection near the site of injection, a known allergy/ hypersensitivity to the material or lidocaine, pregnancy and anticoagulant therapy, it is important for a full medical history to be taken before treatment.8 As noted in the guidelines by the Aesthetic Complications Expert (ACE) Group World, a history of allergic reaction to wasp or bee stings represents an increased risk of allergic reaction to hyaluronidase and should be considered as a relative contraindication, so it’s my personal preference to avoid treating patients with dermal fillers.9
Practitioners should also be aware of medications that predispose to bruising which include painkillers, non-steroidal anti-inflammatories, anticoagulants or vitamin E.10 Practitioners should also be aware of patients who are using isotretinoin. There are divided opinions as to whether this drug for acne treatment affects dermal fillers. It has been advised in the literature not to inject dermal fillers for at least six months following cessation of isotretinoin.11 This recommendation is challenged, and some clinicians believe that the drug has no effect on outcomes and are happy to use dermal fillers while the patient is undergoing this medication, as there is no conclusive evidence.12 Personally, I will be cautious and wait six months before treating the patient.
It is important for practitioners to have a strong anatomical knowledge and understand the properties of the product being used to maximise the efficacy of the treatment as well as minimising complications.13 The temporal region is based on a bony platform consisting of the parietal, frontal, sphenoid and temporal bones. The overlying soft tissues are arranged in layers, which contain the temporal neurovascular structures.5 The temples form the lateral boundary of the periorbital region of the upper third of the face.14
The temporalis muscle is a large, flat muscle that lies within the temporal fossa of the skull. This fan-shaped muscle arises from the entirety of the temporal fossa below the temporal line, as well as the deep surface of the temporal fascia.15 Its muscle fibres converge anteriorly to form a tendon, which runs deep to the zygomatic arch. The tendon inserts on the apex and medial surface of the coronoid process, and the anterior border of the ramus of the mandible.15
In the temporal region, the blood supply is acquired from the superficial temporal, middle temporal, deep temporal, posterior auricular, transverse facial, zygomatico-orbital, zygomaticotemporal, zygomaticofacial and middle meningeal arteries.16 Branching off the maxillary artery in the infratemporal fossa, it travels through the foramen spinosum to supply the dura mater and the calvaria, which is deep.16
The superficial temporal artery supplies the temporal and parietal area, which originates in the parotid gland. This runs superficially upward along the vein and the auriculotemporal nerve, between the ear tragus and the posterior root of the zygomatic arch. It then divides into two branches: the frontal branch and the parietal branch.17 As a result, these vessels and nerves are not, theoretically, at risk if the practitioner refrains from injecting past the lateral safety line.17
The sub-temporalis space is the safe area for dermal filler injection, located in the upper area of the temporal region adjacent to the frontal border. Whilst inferior to the middle temporal vein and near to the zygoma, the superficial temporal fat pad is the targeted area for safe injection.18

I use hyaluronic acid-based dermal filler products because of the hydration effect that we encounter and the ability to reverse these fillers. These products are temporary, but practitioners can expect results to last between six to 12 months. Practitioners should consider the different viscoelastic, elastic modulus, cohesivity, hyaluronic acid concentration and viscosity properties.19-21 For treating the temples, I prefer to use plastic surgeon Dr Arthur Swift’s technique to address volume loss by using a product with a large particle size, to restore volume, and a high G prime, to help with lifting.22
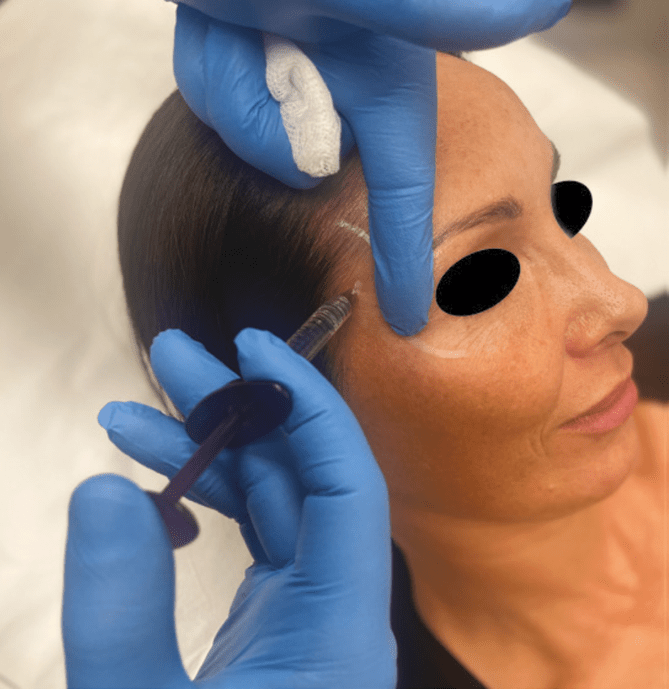
I prefer the multi-layer approach to gain the maximum result and optimise product usage.22 My approach is to insert a deep vertical depot high up in the thinner fibres of the temporalis muscle.23 It is important to ensure that you are on the bone with a needle, and secondly a deep horizontal depot with a cannula. I use the TSK Laboratory 25 gauge, 50mm cannula.
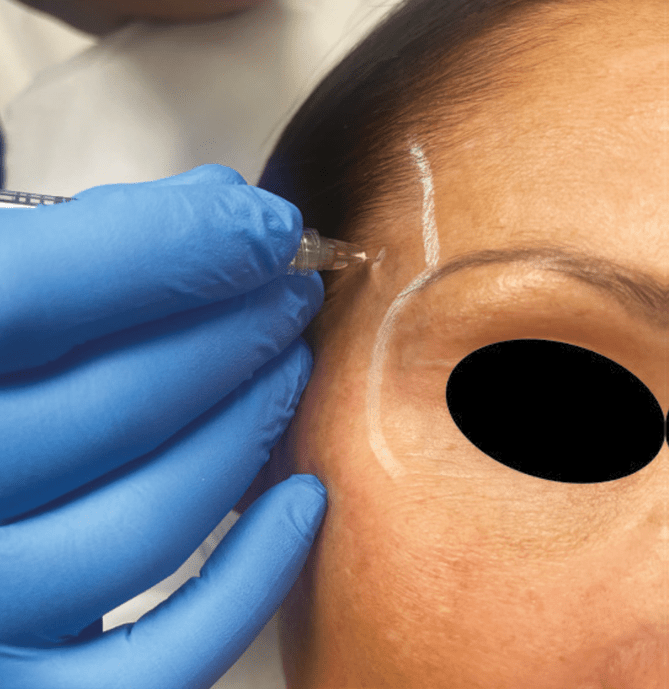
Personally, I use Dr Swift’s technique to address volume loss, however, I’m aware of there being up to eight different techniques which practitioners can use to treat the temples.22 The injection technique for the temples is injecting 1cm up from the lateral orbital rim and 1cm lateral to the temporal fusion line, high up in the thinner fibres of the temporalis muscle. The depth here is 4mm before you hit bone.23 Again, ensure that you are on bone, as you may puncture an artery or vein that you couldn’t palpate. As with all filler treatments, there are risks of complications, such as bruising, swelling or vascular occlusion which can, in extreme cases, result in blindness.24,25 On the temporal bone in this region there are no vessels of concern, as the terminations of the deep temporal arteries are small and posterior. I advise keeping a finger medial to the injection point while injecting so the product doesn’t diffuse medially.
It’s rare that I use more than 0.5ml of product here. I chose a higher G prime product, as it will try to lift and hit the undersurface of the deep temporal fascia, spreading between it and the muscle. You can see the product flowing towards the zygoma.22 I prefer to leave the temple area flat after injecting and not convex, as I’m trying to recreate a triangle of youth and a V-shaped outline would require flat temples.
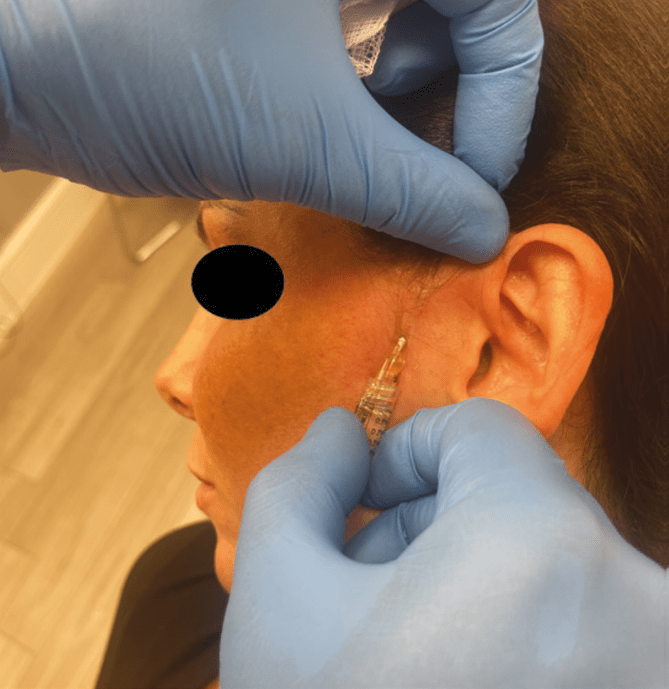
The result with this technique is to soften the transition from the upper face to the mid-face. I use a 23 gauge needle for the insertion point, 1cm anterior to the tragus. I’ll then use a 22 gauge cannula with a high G prime HA filler. I inject subcutaneously into the subdermal plane. There are no major arteries located here so I inject into the temporal hairline, close to the lateral border of the eye and place 0.2-0.5ml of filler per side.26 Adjunct treatment may include toxin around the orbicularis oculi as well as fillers laterally to lift eyebrows or for mid-facial volumisation. This creates a result where the volume loss is restored and temporal lifting has taken place.
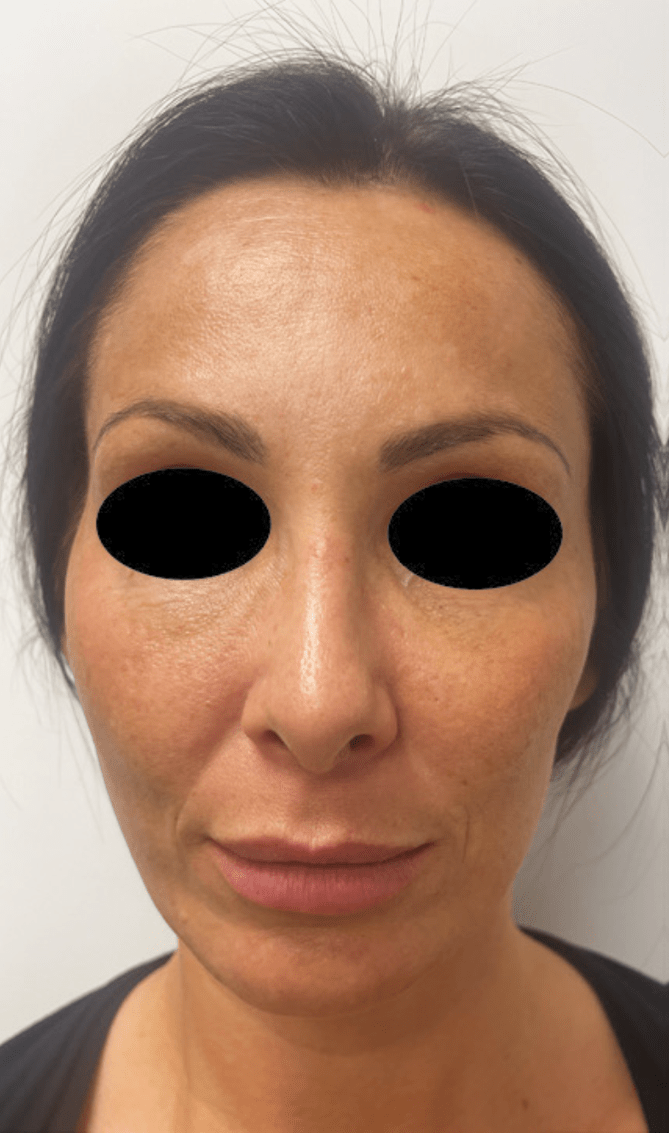

Treating the temple can have impactful results for patients experiencing the signs of ageing. There are several techniques that practitioners can choose from. It’s important to identify the suitable patient and the underlying cause of the deformity. This allows you to choose not only the appropriate product, but the suitable technique too. Despite this, the temples are a highly skilled and advanced procedure to treat and should be undertook by trained practitioners with many years of experience.




